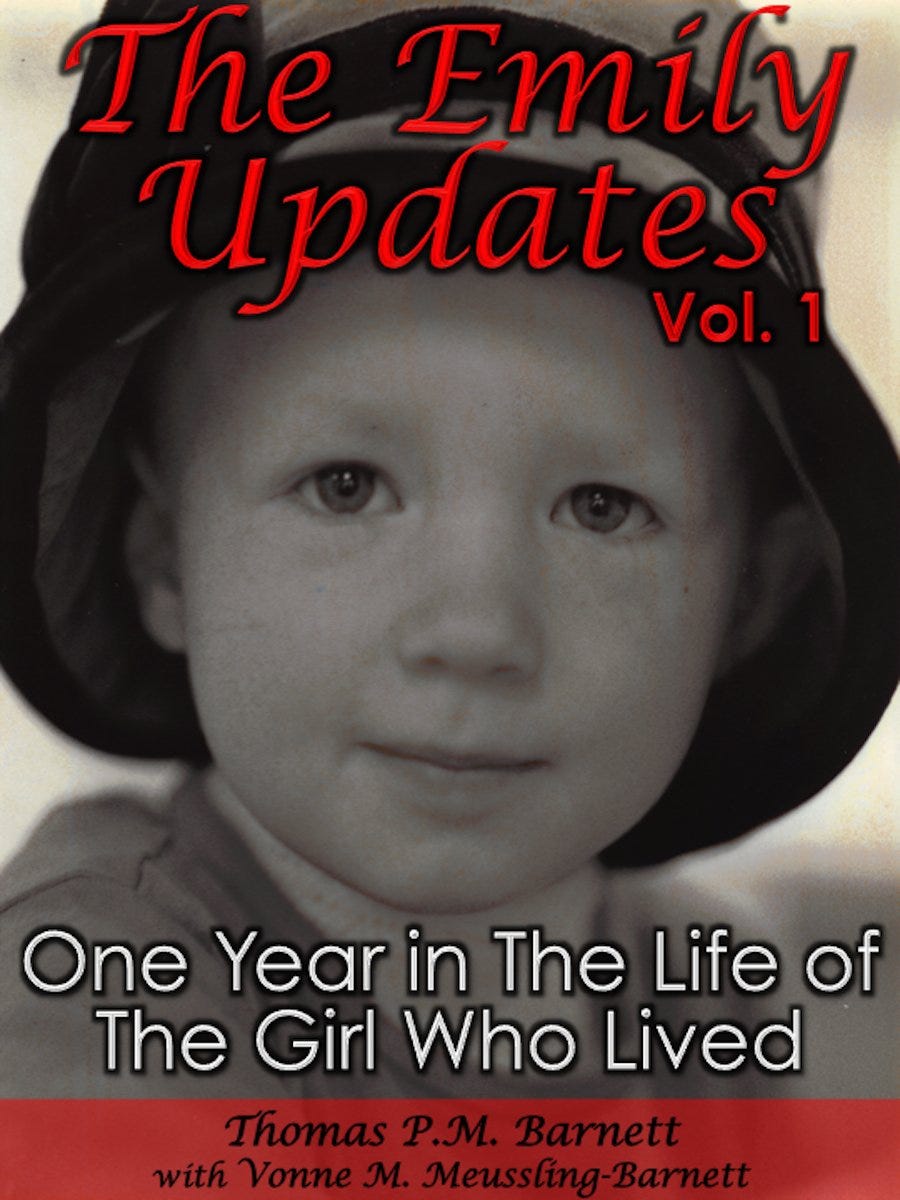
Serial 3:11 of "The Emily Updates"
Sharing a 30-year-old diary of my firstborn toddler's cancer battle
Chapter 2 (continued)
The Past as Prologue (II): Descent
Sunday, July 10th (Day 3)
Sunday starts out very quietly. We’re all a bit puffed up about Em’s amazing effort at getting through all that surgery, especially coming on the heels of all those nasty diagnostics. All vital signs point to our discharge from PICU by the end of the day, and that alone is cause for rejoicing, as all the doctors and nurses beamingly confide.
“She’s one great fighter all right,” says one PICU nurse.
Still, to celebrate much at this point would be like the D-Day soldiers laughing it up big- time on Normandy Beach that evening. Sure, it’s great to still be alive, surviving the deadly assault, but so much danger lies ahead. Conflicting interpretations of the CAT Scan still abound: are those dark areas in the lungs metastasized Wilms’ Tumor? Bits of collapsed lung? Old scars? Nobody knows.
The question of which stage diagnosis Emily receives is crucial because there’s a wide variance in treatment protocols and, naturally, a significant variance in historical odds. If the Wilms’ is seen as remaining solely within her right kidney sack, we’re talking Stage II, and that means chemo for less than a year with no radiation. If the Wilms’ has escaped the kidney sack and moved into surrounding tissue, then we’re talking Stage III, or anywhere from a year to 15 months of chemo with abdominal radiation on the side where the kidney was removed. If the dark spots in the lungs are metastasized Wilms’, then it’s Stage IV, with the same Stage III treatment regimen plus radiation to both lungs.
Now, Hoy suspects some of the abdominal lymph nodes are infiltrated, so it seems we’re already in Stage-III territory. Therefore, the question of the lung spots determines how much radiation she’ll receive: either just one side of the abdomen or her entire chest as well. The difference is huge, because when you radiate the lungs, you nail the heart too.
Of course, there’s still the formal pathology, the results of which remains days away. If the histology (tissue structure) is unfavorable – otherwise known as anaplastic (the worst type, where the cells display an almost devolved lack of differentiation) – then chances are she’ll die, as success rates with that type are dramatically lower.
So only so much pride can be purchased by Emily’s courageous performance to date. Your head is just too crowded with the guilt of discovery and fear of the future to let much else in.
On a practical level, much of our interaction with staff concerns Em’s pain medication and the removal of various tubes running into her. Emily clearly wants the Foley catheter out pronto, as she asks to have her diaper put back on as soon as she is coherent enough to realize her situation. It quickly approaches near-constant pleading on her part, as the catheter is the number one limit on her mobility in bed. Naturally, she hates the nasogastric tube as well, but the diaper remains her most persistent demand through that first recovery day. Both tubes are removed by early afternoon, but there’s a lesson to be had in this process.
That lesson is: ask, ask, and ask again. The decision to remove such painfully intrusive tubes cannot be made by floor nurses. If you choose to wait on the good doctor’s grand appearance, well, you can wait all day and deep into the night – especially on a Sunday. Answer? Keep bugging the nurses and floor residents until they, in turn, bug the chief nurse and chief resident. Then you move your nagging up a notch until the chief nurse and chief resident start calling the surgical residents. When they appear, start on their case immediately. If they hem and haw about needing the surgeon’s permission, then stomp off toward the unit secretary, demanding loudly that the surgeon be paged immediately. At that point the resident will probably stop you and say they’ll get an answer within an hour. Then you simply start the ladder-process all over again about checking on the surgeon’s response. Point being, the hours of extra agony that you slice off by pushing this decision make a huge difference in your child’s comfort and thus recovery. Em brightens up considerably with diaper on and nose tube out.
We’re not pushing the envelope of medical necessity – but of medical bureaucracy. In doing so, we’re simply – and smartly – building on our growing reputation as parents who aggressively co-manage their child’s care. Think of Shirley MacLaine’s mother character in “Terms of Endearment.” Co-managing is not an exaggeration, as there’s lots of wiggle room in any hospital procedure or service. The big thing is not being afraid to ask. Moreover, it feels good. Our aggressive advocacy mitigates our grief of a past-life lost, the guilt of the current situation still unfolding, and the fear of a highly uncertain future.
Having increased Emily’s fragile comfort level, things go wrong on another level shortly after noon. The morphine they’re giving her to handle the intense pain is producing a nasty side effect. Every so often, after the narcotic sends Em off to the lala-land of light sleep, she’s abruptly awakened with a terrifying startle that literally lifts her off the bed – “Exorcist”-style. It’s scary to watch: a body-slamming version of the startle most of us know from light sleep. This rendition, however, is a nasty, jerk-contraction of every muscle in her body. Her head pulls forward off the pillow, arms and legs shoot out in all directions, and her torso lifts off the mattress for a split-second. All this lightning-flash movement sends Em into spasms of pain, given all her sutures. So she awakens, starts weeping plaintively, and the morphine submerges her once again just below the waterline of consciousness. Then POP! It happens again.
God that child cries out so, the pain as much emotional as physical. It seems like this cruel trick the morphine’s playing on her.
Rest little girl, I’ll take care of you. There, there now . . . SLAP! Got you, didn’t I? That’ll teach you for dropping off! Now, now, I’m sorry. Please, little girl, go back to sleep. Just relax and let me do all the work. Yes, little darling, sleep.
Seeing Emily pop off that bed again and again sends Vonne and I into utter despair. The nurses’ first answer is to pump up the volume, saying they’re loath to switch meds since Hoy dictated morphine, and he’s considered a near-god by nurses and residents alike. His preferences are not easily challenged via the staff, although he seems quite flexible with us – the parents. The weird thing is, Hoy is big on bringing the patient back up from surgery ASAP, which makes everyone’s deference to this numbing morphine regime all the more strange in our eyes.
Finally around 2pm, after seeing Em lift off the bed once again as though some invisible force is tossing her around, Vonne and I start taking turns lying in bed and physically pinning her down so the startles don’t shake her so painfully. It works to a certain extent, and she calms down some. But this is a Band-Aid solution for one major-league wound. In short, it sucks.
It’s at one point when I was lying next to Em that good family friend Vickie Sands appears with daughter Michaela to visit and bring us stuff from home. Vickie and her husband Jeff, a colleague of mine, are taking care of our house while we're stuck here. Four-year-old Michaela looks pretty scared, but she puts on a brave face for Emily, who's still weeping from the last jerk-around. I’m lying next to Em, covering as much of her body as possible with my free arm and leg and kissing her head – and feeling awfully pathetic in front of these close friends. It’s simply being confronted with the yawning gap that’s so instantaneously opened up between them and us. Only hours before we’d shared the same lives.
Grateful as I am for the visit, it leaves me intensely sad and angry. Vickie drives Michaela back home on this beautiful summer day, the kind when we often get together as families and hit some local park. Michaela goes home to her toys, her little brother Daniel, and her own bed. Meanwhile Em and I lie together crying, holding each other tightly, and hoping the next spasm stays away just a couple minutes more. All the time we’re waiting to find out if this effort is just a cruel hoax and she’ll die soon anyway. I feel so angry with this stunning turn of events, this seemingly capricious judgment from on high that sentences us to this fate and leaves others – standing just to our right and left – to walk away untouched, that I’m ready to denounce, desecrate and destroy everything anyone holds dear in this life. My soul is so black right now that I feel I understand every evil act ever committed. More than that, I covet them.
Imagine pissing me off this afternoon.
Later in the day we’re discharged from PICU and we simply wheel Emily’s bed past the main elevators and into the so-called Step-Down unit known as C53.
The morphine spasms worsen. Everyone is talking about it, but no one is doing anything to stop them. After a while we press them about alternatives. I can’t help wondering: What's the goddamned Rubicon between morphine and the rest of the pharmacological universe anyway! Finally, a nice nurse, the aptly named Mary Paine, mentions Toradol. It’s a non-narcotic with few side effects and it often works wonders without doping the patient too much. Good God! This sounds just like what Hoy would want!
We continue badgering the staff, verbally beating up floor residents and working our way up to the chief resident – one talented but snotty lady who acts like parents are the biggest pain in the ass any doc can imagine. She wants all sorts of vitals taken – over and over again. This triggers the great blood pressure fiasco.
Hospitals have these glorious devices that take blood pressure automatically every few minutes. They are not built for little kids, however, who – besides often simply being too small – tend to squirm about and throw the readings off. Well, they strap one on Em even though we tell them that it frightens her and they're likely to get falsely high readings. Chief resident Kiss-My-Ass says it's imperative to get a correct reading, “So keep trying the machine until we get one!” Pretty soon Em is hysterical, so her blood pressure shoots up.
Then the room fills up with doctors, residents, and nurses – everyone but Waldo. Everyone is babbling about Em’s dangerously high blood pressure: “She seems so spooked by people! Maybe we need another reading! If we can’t get it down we’ll need to take drastic action!”
Then we go ballistic. I start into the chief resident. Nona Vonne is yelling that there are too many people in the room, getting so mad that Granddad Carl jerks her outside before she hits someone. Vonne rips off the blood-pressure cuff. Finally, Kiss-My-Ass relents.
[Cut to exterior shot of hospital room: doctors and nurses exit en masse, the chief resident mumbling to herself about “asshole parents.” Seconds later the blood-pressure machine comes spinning out. The door slams. The lights inside go out. All is quiet. Cue the tinkling piano score.]
They never again use the blood-pressure machine on Emily during our hospital stay. From that point on we carry with us a manual version with an extra-small cuff. Anyone trying to wheel in the machine is stopped at the door and told, “No thanks.”
We have many run-ins with the chief res until she realizes we aren’t going to back down whenever she pulls out her I’ve-got-my-ship-to-run crap. Her chart notes about us are a masterpiece of understatement: “Parents seem to feel more in control when given sufficient information regarding procedures and policies.”
Yeah. Uh-uh.
Well, push comes to shove and we finally get hold of Hoy’s No. 1 surgical resident, the inimitable Dr. Petro. She’s obviously talented, but her personal warmth registers just north of zero degrees Kelvin. She makes Kiss-My-Ass seem downright bubbly in comparison. She thinks Emily’s blood pressure is due to pain, not the morphine. Just like that, she comes to this rapid-fire conclusion.
Apparently our detailed and highly graphic descriptions of the spastic tremors come off as so much hysterical parenting. She just frowns at us. “Never heard of it,” Petro says. “It’s not possible.” Hoy specified morphine, so how can we expect his right-hand disciple to call her rabbi wrong. Get real, hysterical parents! But okay, she announces with a withering look, I’ll disturb the great man!
Petro comes back about an hour later. Seems Hoy approves the switch to Toradol in nothing flat. His only concern is that Toradol reduces white counts if used over a substantial period, but that’s not likely here. “So get on with it!” he says.
It's now 10pm. We’ve been begging for this change for eight hours. Nurse Mary Paine gives Em a “loading,” or double dose, of Toradol.
A little less than two hours later Emily is sitting up in bed, smiling, talking and playing with toys. She’s asking for stuff to drink and eat, but she’s still Nothing Per Oral.
Anyway, the transformation is beyond stunning. One hour she’s writhing in pain and delirious, triggering the whole blood pressure fiasco with the cast of thousands. The next, she’s relaxed and calm. We watch videos and play with some toy animals that Nona Vonne bought. Life is back to some semblance of normality. Everyone is being nice to one another again. The chief resident and I engage in pleasant small talk. I tell her I’ll call her “Dr. Henry” if she’ll stop calling me “Dad.” Residents love to hear the title.
We finally talk Em-Cat into sleep around 1am. Nona and Carl head off to the Leavey Alumni Center, where they’ve got a room. We have a cot brought for Vonne and a recliner for me. We’re reminded that only one parent can stay, but we just smile and thank people profusely for that timely insight into hospital procedure. Then we escort them to the door and shut it behind them.
As Emily drifts off to sleep, the spasms return. There’s still a lot of morphine in her system. We lay her on her stomach and surround her with pillows. Then I sleep next to her with my arm and leg pinning her down. This way, when she’s startled, she simply reflexes into the pillows, feels the reassuring weight of my limbs, and drifts back to sleep without the crying jag. About 4am the jerking finally stops, whereupon Em pointedly asks me to leave her bed.
I try the recliner for about five minutes and then sneak onto the empty bed on the other side of our double room. The night nurse bounces me at 6am.
“Hospital rules, you know.”
Monday, July 11th (Day 4)
Things settle down a lot this morning. We make our peace with the nursing and resident staffs. They understand us now, we understand them, and mutual respect emerges amidst the shared experiences. We know they’re doing great by Em. We never doubt that. Conversely, they come to appreciate what assets we are in Emily’s care. She’s one kid they never have to worry about. Someone is always with her, meeting her needs, voicing her requests, sheltering her from the din. Once both sides get used to the other’s style and requirements, things smooth out significantly.
The blood draw this morning shows Em came through surgery just fine. She’s holding her weight, despite losing that two-pound kidney. Her chart notes describe her recovery with code phrases like “MAE” [moves around easily] and “OOB [out of bed] ambulatory in the hall with parents without difficulty.” She’s still forbidden to eat or drink through the morning, but receives permission for sips of liquids in the afternoon. It’s the first thing to pass her lips since Friday night. One nurse’s notes describe Em as “playful, somewhat cheerful, coloring in bed but became fretful when approached.” She also notes that it’s hard to listen for bowel sounds in her abdomen because Emily cries when she tries with the stethoscope.
Before lunch Dr. Gootenberg stops by with his residents: the charming Victor Alidow, who falls so hard for Emily that he brings her a teddy bear; and Elizabeth Sutton, also a sweetheart. Perhaps residents just get softer when they rotate to peds onc. Anyway, we prefer them to the stone-faced, laconic surgical crew.
Gootenberg assumes that the lung spots found on the CAT Scan are metastasized Wilms’ Tumor. He quickly outlines possible biopsy routes, stressing that the ultimate choice resides with the surgeon Hoy. Feasibility is determined not just by ease of access, but also by the time crunch of starting the treatment protocol – i.e., radiation and chemotherapy. For example, the simplest method is by needle insertion, but the odds of getting enough material – and thus conclusive data – are only so-so. More invasive methods carry other risks, of course. But the bottom line is this: the protocol calls for chemo within ten days of kidney removal. Historical studies show that, once you go past ten days, survival rates drop significantly.
We’re already on the clock.
Gootenberg talks at length about the National Wilms’ Tumor Study Group, which was established in the late 1940s. The treatment protocol was formalized in 1969 – one of the first for cancer. Since then, the NWTS (known affectionately as the Nitwits – those wacky oncologists!) has been run by a national board that actively oversees most Wilms’ cases in the country (about three out of every four). The NWTS is currently in its fifth seven-year study of the treatment protocol, the disease itself, and long-term survivorship.
As Gootenberg explains, Emily is in a rather unusual situation. Her lung nodes are not picked up on the chest X-ray, but are barely visible on the CAT Scan. Now, the Nitwits know that, in the past – before the advent of the more powerful CAT Scans, they must have treated a few kids as Stage-III cases (no spread above diaphragm) when they were really threshold Stage-IV (spreading to lungs). So they’re sort of undecided, protocol-wise, regarding the value-added of radiation to the lungs when patients are right on this diagnostic borderline. Why? You don’t radiate some kid’s heart and lungs on a whim; the payoff has damn well gotta be there. In the fourth NWTS study, approximately 40 kids fell into this in-between category, and when left to the preferences of their attending oncologists, half went Stage III and half went Stage IV. Of the twenty in each group, one died in Stage IV and two died in Stage III – not a significant difference. So the issue of the treatment protocol is still up in the air as far as the Nitwits are concerned.
Gootenberg’s attitude: “We have one good swing at the bat. If we kill it right away, Em has probably got it beat – for good. To go light on treatment risks striking out completely. Better to hit it out of the park with the bigger bat.”
To paraphrase F. Scott Fitzgerald, there are few successful second acts with Wilms’ Tumor. Relapses trigger much harsher protocols featuring survival rates far south of 50 percent. Having stated his philosophy, Gootenberg stresses that it’s too early to make this decision. We’re still waiting on the pathology.
Lombardi peds-onc art therapist Tracy Councill stops by. We first met Tracy on Friday, when she gave Em some markers to kill time before the surgery. Tracy promises to keep Emily supplied with crayons, markers, and Play-Doh throughout her time in the hospital. Today she also brings over the sand table from the clinic for Emily to play in – right off the side of her bed. Em-Cat enjoys it so much that, by day's end, Nona is already talking about having Granddad Carl build one. Tracy says she'll alternate with another lady, named Lynn, during the weekdays, and judging by this charming woman's way with Emily, both Vonne and I can see what an important role these two artists will play in the days ahead. Tracy's visit is a nifty release for us all. With Lombardi, we sense a larger support structure at work. These people operate off a bigger picture, and we need anchor points right now.
Em gains strength as the day progresses. That night, around nine, she ventures into the playroom down the hall. Less that 48 hours after having her kidney removed, Emily climbs up the Little Tikes slide and down she goes before we can react! Later that evening she has her last Toradol. From that point on, it’s just Tylenol for Emily. Both doctors and nurses are simply amazed at her recovery and ability to handle pain. “Resilient” doesn’t come close to describing the feat.
That night Vonne sleeps on the cot in the room, while I try the parent’s lounge. I find it too spooky and sneak into bed with Emily, who lets me stay all night this time. Granddad and Nona stay at the Leavey Center again.
Tuesday, July 12th (Day 5)
Nona Vonne and Granddad Carl leave this morning, and we’re sorry to see them go. They had gone to such great lengths (pun intended) to be at our side during the worst hours after surgery, showering us with attention and support every minute. It's hard to imagine what it all would have been like if they hadn't been here for us.
Gootenberg sweeps in with important news: after re-evaluating the CAT Scan, the radiologist identifies the lung masses as suggesting Wilms’ metastases. He goes on to say that he wants an oblique chest X-ray done to get a better look at the nodes, but Vonne and I stop listening at this point, so stunned are we by the bad news. So far, every time we've come to some fork in the road, we get shoved down the dark path. Gootenberg’s request for a nuclear bone-scan of Em's entire body goes in one ear and out the other. Our throughput channels are simply overwhelmed at this point.
A bit later we have our first long talk with Yvonne Bush, our Lombardi-assigned social worker. She enters a fairly detailed description of our backgrounds in Emily’s chart, as well as a listing of our concerns. As she notes, “Both parents have mentioned that this is a huge change in their expectations and plans. They have voiced that this will take some time to adjust to.” She writes that we’re relieved when Gootenberg tells us how hard it is to detect this cancer, because we feel guilty for not picking it up earlier. She ends with, “Family seems very capable in working with complex systems and has excellent self-awareness, insight, and ability to problem-solve.”
Any wonder why we like Yvonne from the start?
Vonne’s brother Todd shows up magically for lunch, juggling his business travel schedule to give him a few hours of layover at Dulles. After spending some time with his niece, he whisks Vonne off for a well-deserved lunch, and it does wonders. Todd is Vonne’s number-one comrade from childhood, and his short stay picks her up tremendously. Coming from the real world, he’s a welcome tonic for us all.
Emily is placed on a regular diet this afternoon, meaning her first solid food since Thursday evening. It makes her feel a whole lot better.
I take Emily down for the chest X-ray in the early afternoon. It’s a real jerk-around. First we have to hustle downstairs with no warning, and then radiology says they’re not expecting us. I unleash my tongue big-time and they say they’ll work us in pronto. It’s a tough shoot, as all the big, noisy machinery frightens Em. For this thirty-month-old tyke, no day passes without some new scary adventure.
Donna Oishi, the head peds onc nurse at Lombardi, stops by and shows Vonne and I how to change Emily’s Broviac catheter bandaging. Like all the peds onc nurses, Donna exudes a confident and upbeat personality. She breezes in and out like she owns the place, oozing can-do attitude. We find ourselves being really impressed, but not sure why. I guess the peds onc nurses represent this tough-but-hopeful future to us. They sweep into the room like angels-of-our-better-future, filling us up with confident thoughts about ourselves and the difficult battles ahead, and then sweep right out again – Mary Poppins-like. Maybe we're just imagining their effect, or maybe they're adept at giving families what they need at time like this. Whatever the reason, we desperately want the peds onc nurses to be special. We feel Emily’s future is largely in their hands.
Emily ends the day with only the telemetry sensor still on her finger. When we leave for a walk, we simply stuff the battery-powered transmitter into the back of her diaper.
At bedtime, a friend from the District, Steve Grundman, treats us to some carryout pizza. Vonne stays at his home for the evening, while I spend the night on the cot.